ORAL COMPLICATIONS OF CHEMOTHERAPY & HEAD/NECK RADIATION AND ITS MANAGEMENT





INTRODUCTION
Oral complications are common in cancer patients especially head and neck cancers.
Oral cavity is at high risk of side effects from chemotherapy and radiation therapy. Some of the reasons are:
chemotherapy and radiation therapy stops the growth of cancer cells and by doing so , it also stops the normal cells lining the cancer.
they also cause changes in mucosal lining , normal salivation and healthy balance of bacteria.
wear and tear.
Preventive measures may lessen the severity of the complications.
LIST OF COMPLICATIONS:
1.Mucositis.
2.Bleeding.
3.Pain.
4.Taste changes.
5.Infections.
6.Dry mouth.( Xerostomia )
7.Dental caries & periodontal problems
8.Jaw stiffness.
9.Osteonecrosis.
10.Tissue & bone loss.
11.Malnutrition.
CLINICAL PRESENTATION OF THESE COMPLICATIONS:
1. MUCOSITIS:
caused by both chemo & radiation therapies.
red, burn like sores or ulcer like.
sites: gums, tongue, buccal mucosa, roof & floor of mouth.
pain, bleeding, super infections & difficulty in eating.
2. BLEEDING: caused by anticancer drugs
bleed from areas of gum disease or from mucositis.
bleeding during brushing, flossing or eating.
may be mild or severe.
sites: lips, soft palate & floor of the mouth.
3. PAIN:
anticancer drugs can damage the nerve.
tooth sensitivity.
pain in jaw muscles.
4. TASTE CHANGES: ( dysgeusia )
may be due to chemotherapy or radiation therapy.
due to – damage of taste buds, dental problems, infections, dry mouth
in chemotherapy patients- spread of drug within mouth.
in radiation therapy – damage to taste buds
changes in sweet, sour, bitter & salty tastes.
5. INFECTIONS:
chemotherapy weakens the immune system.
mucositis & dry mouth further causes infections.
(i) Bacterial infections:
- gram positive and gram negative cocci infections.
- periodontal disease and dental caries.
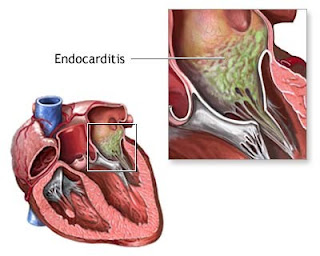
- may complicate endocarditis in valve disorders.
(ii) Fungal infections:
- common in patients under radiation therapy.
- antibiotics & steroids are often used by patients under chemotherapy, which changes the bacterial balance in the oral cavity fungal infections.
- deep fungal infections.
- candidal infections.
(iii) Viral infections:
- herpes virus infection
6. DRY MOUTH ( Xerostomia ):
occurs as a result of salivary gland destruction on radiation therapy.
thick stringy saliva
difficulty in speech, swallowing & taste.
burning sensation.
thirst, halitosis.
cuts & cracks in lips.
dental caries & periodontal diseases. leathery tongue.
7. Dental caries & periodontal diseases:
due to xerostomia, bacterial infections, radiation induced .
8. Jaw stiffness:
a long term complication of radiation therapy characterised by development of fibrosis leading to difficulty in opening the mouth.
9. Osteoradionecrosis:
Radiation therapy --> end arteritis --->tissue hypoxia -->
-->hypocellularity -->devoid of fibroblast , osteoblast
and osteo competent cells
- Pain
- Swelling
- Trismus
- Exposed bone
- Pathologic fracture
- Oral-cutaneous fistula formation
10. Tissue and Bone loss:
radiation therapy causes it.
when soft tissue death occurs -->ulcers form -->grows ->> -->>pain -->infections
when bone loss occurs --> pathological fractures.
11. Malnutrition:
due to:
- side effects of drugs like nausea, vomiting.
- sores in the mouth, dry mouth & pain
MANAGEMENT
PREVENTIVE MEASURES
Eating well balanced diet.
Proper oral hygiene.
Preventive oral health examination:
It consists of checking the following:
mouth sores & infection.
tooth decay.
Gum disease.
Dentures that do not fit well.
Problems moving the jaw.
Problems with the salivary glands.
1. Routine oral care:
- good oral hygiene reduces the complications.
- following are the guidelines:
tooth brushing:
Choose toothpaste with care:
Use a mild-tasting toothpaste;
flavoring may irritate the mouth.
If toothpaste irritates the mouth,
brush with a solution of 1 teaspoon of salt added to 4 cups (1 quart) of water.
Use a fluoride toothpaste.
Rinsing :
Rinse the mouth 3 or 4 times while brushing.
Avoid rinses containing alcohol.
One of the following rinses made with salt and/or baking soda may be used:
1 teaspoon of salt in 4 cups of water.
1 teaspoon of baking soda in 1 cup (8 ounces) of water.
½ teaspoon salt and 2 tablespoons baking soda in 4 cups of water.
An antibacterial rinse may be used 2 to 4 times a day for gum disease. Rinse for 1 to 2 minutes
If dry mouth occurs, rinsing may not be enough to clean the teeth after a meal. Brushing and flossing may be needed.
Flossing :
Floss gently once a day.
Lip care :
Use lip care products to prevent drying and cracking.
2. Oral mucositis :
Swishing ice chips in the mouth for 30 minutes may help prevent mucositis from developing in patients who are given fluorouracil.
Routine Oral care:
dil. Hydrogen peroxide rinses
Kaolin-pectin, aluminium hydroxide & sucralfate.
Lip lubricants like lanolin.
Relieving pain:
Try topical medications for pain. (topical NSAIDS)
Topical anesthetics
Capsaicin & zinc supplements.
3. Bleeding :
Hemostatic agents.
Rinsing with a mixture of one part 3% hydrogen peroxide to 2 or 3 parts saltwater solution (1 teaspoon of salt in 4 cups of water) to help clean oral wounds. Rinsing must be done carefully so clots are not disturbed.
4. Pain :
Topical anesthetic
Analgesics & anti inflammatory drugs.
Antimicrobial.
Anticonvulsant.
Anxiolytic & antidepressants.
Muscle relaxant.
5. Taste changes:
zinc sulfate 45 mg by mouth 3 times/day
Taste buds recover after 6-8 weeks.
6. Infections:
Bacterial infections:
Medicated and peroxide mouth rinses.
Brushing and flossing.
Wearing dentures as little as possible.
Antibiotics.
Fungal infections:
mouthwashes and lozenges that contain antifungal drugs.
Topical antifungal agents. Eg, CANDID mouth paint.
Systemic antifungal drugs for deep fungal infections.
eg, Tablet- ketoconazole 200mg/day
Viral infections:
Antiviral drugs.
7. Xerostomia :
The following rinse may be used to neutralize acid and dissolve thick saliva:
½ teaspoon salt and 2 tablespoons baking soda in 4 cups of water.
A dentist can provide the following treatments:
Solutions to replace minerals in the teeth.
Rinses to fight infection in the mouth.
Saliva substitutes or medications to stimulate the salivary glands.
Fluoride treatments to prevent tooth decay.
8. Dental caries & periodontal diseases:
operative care & topical fluorides.
Proper oral hygiene.
9. Jaw stiffness:
Physical therapy.
Pain treatments.
Medication
10. Tissue and bone loss:
Wearing removable dentures or appliances as little as possible.
No smoking & No consumption of alcohol.
Using topical antibiotics.
Undergoing surgery to remove dead bone
hyperbaric oxygen therapy.
11. Malnutrition :
High calorie, high protein
nutritional juices.
Enteral tube feeding.
Vitamin and mineral supplements.
12. Osteoradionecrosis:
Medical therapy in treatment of ORN is primarily supportive, involving nutritional support along with superficial debridement and oral saline irrigation for local wounds
Hyper baric oxygen.
Surgery.
CONCLUSION
Oral and dental care is important in all phases of treatment of patient with head and neck cancers, especially preventive measures are to be considered a lot


Comments