infective endocarditis & its dental prophylaxis..



Definition
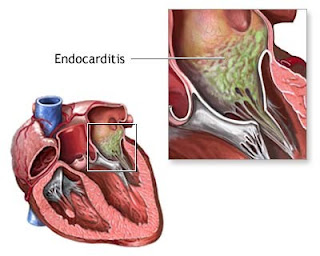
Subacute Bacterial Endocarditis (SBE) is a bacterial infection that produces growths on the endocardium (the cells lining the inside of the heart). Subacute bacterial endocarditis usually (but not always) is caused by a viridans streptococci (a type of bacteria); it occurs on damaged valves, and, if untreated, can become fatal within six weeks to a year.
Description
Endocarditis has traditionally been classified as acute or subacute based upon the pathogenic organism and the clinical presentation. This distinction has become less clear, however, and the less specific term "infective endocarditis" is now more commonly used. Most patients who develop infective endocarditis have underlying cardiac disease, although this is frequently not the case with intravenous drug abusers and hospital-acquired infections. Important factors that determine the clinical presentation are:
1.the nature of the infecting organism
2.whether the infection is superimposed upon preexisting abnormal cardiac structures
3.the source of infection, since endocarditis in intravenous drug abusers and infections acquired during open heart surgery have special features
More virulent organisms, Staphyloccus aureus in particular, tend to produce a more rapidly progressive and destructive infection. Patients are more likely to present with:
#fever
#early embolization (vegetation dislodging from the heart valve and traveling through the blood stream)
#acute valvular regurgitation (back flow of blood in the heart)
#abscess formation (pocket of infection)
Streptococcus viridans, enterococci, and a variety of other bacteria and fungi tend to cause a more subacute form of endocarditis. Streptococcal infection tends to be more chronic, though the average incubation period is 1 to 2 weeks.
Causes
Subacute bacterial endocarditis (SBE) is usually caused by streptococcal species (especially viridans streptococci), and less often by staphylococci. SBE often develops on abnormal valves after asymptomatic bacteremias (bacteria traveling through the bloodstream) from infected gums, or from gastrointestinal, urinary, or pelvic procedures.
Symptoms
Most patients present with a fever that lasts several days to 2 weeks. Nonspecific symptoms are common. Cough, shortness of breath, joint pain, diarrhea, and abdominal or flank pain may be present. About 90 percent of patients will have heart murmurs, but murmurs may be absent in patients with right-sided heart infections. A changing murmur is common only in acute endocarditis.
Diagnosis
Endocarditis is suspected in a patient with a heart murmur and unexplained fever for at least one week, and in an intravenous drug abuser with a fever, even in the absence of hearing a murmur. A definitive clinical diagnosis requires blood cultures that grow bacteria. Echocardiography (ultrasound study of the heart) may visualize vegetations (growths) on heart valves.
Treatment
Cure of endocarditis requires eradication of all microorganisms from the vegetation(s), usually on the heart valve. Bacterial endocarditis almost always requires hospitalization for antibiotic therapy, generally given intravenously, at least at the outset. Most patients respond rapidly to appropriate antibiotic therapy, with over 70 percent of patients becoming afebrile (without a fever) within one week. Occasionally, therapy with oral antibiotics at home will be successful. Antibiotic therapy must usually continue for at least a month. In unusual cases, surgery may be necessary to repair or replace a damaged heart valve. Complications If bacterial endocarditis is not adequately treated, it can be fatal. This is dependent on the infecting organism. Even when treated, further damage to a heart valve may can to heart failure. In addition, blood clots can form and travel throughout the bloodstream to the brain or lungs.
Prevention
It is important that you tell your dentist or physician about any risk factors you may have for endocarditis. People with predisposing factors for bacterial endocarditis are those with:
prosthetic heart valves
previous bacterial endocarditis
congenital heart disease
rheumatic valve dysfunction
hypertrophic cardiomyopathy
mitral valve prolapse with valvular regurgitation
If these predispositions are present, the patient should be given antibiotics before most medical or dental surgeries and whenever any significant skin infection occurs. Your physician will recommend which antibiotic(s) to take before, and in some cases, after your procedure.
Endocarditis prophylaxis recommended
1. Dental extractions
2.Periodontal procedures, including surgery, scaling, root planing, probing and recall maintenance
3.Dental implant placement and reimplantation of avulsed teeth
4. Endodontic (root canal) instrumentation or surgery only beyond the apex
5. Subgingival placement of antibiotic fibers or strips
6.Initial placement of orthodontic bands (but not brackets)
7. Intraligamentary local anesthetic injections Prophylactic cleaning of teeth or implants, where bleeding is anticipated
Endocarditis prophylaxis not recommended
1.Restorative dentistry (operative and prosthodontic), with or without retraction cord
2. Local anesthetic injections (nonintraligamentary)
3. Intracanal endodontic treatment (post-placement and build-up)
4.Placement of rubber dams
5. Postoperative suture removal
6.Placement of removable prosthodontic or orthodontic appliances
7.Oral impressions ,Fluoride treatments, Oral radiographs
8.Orthodontic appliance adjustment
9.Shedding of primary teeth
Prophylactic regimen that is proposed by AHA
Standard general prophylaxis
1.Amoxicillin
Adults: 2 g Children: 50 mg per kg Taken orally one hour before the procedure
Patient is unable to take oral medications
1.Ampicillin
Adults: 2 g Children: 50 mg per kg Given IM or IV within 30 minutes before the procedure
Patient is allergic to penicillin
1.Clindamycin (Cleocin)
Adults: 600 mg Children: 20 mg per kg Taken orally one hour before the procedure
2. Cefadroxil (Duricef) or cephalexin (Biocef, Keflex) †
Adults: 2 g Children: 50 mg per kg Taken orally one hour before the procedure
3. Azithromycin (Zithromax) or clarithromycin (Biaxin)
Adults: 500 mg Children: 15 mg per kg Taken orally one hour before the procedure
Patient is allergic to penicillin and is unable to take oral medication
1. Clindamycin
Adults: 600 mg Children: 20 mg per kg Given IV within 30 minutes before the procedure
2. Cefazolin (Ancef, Kefzol)
Adults: 1 g Children: 25 mg per kg Given IM or IV within 30 minutes before the procedure


Comments
I have taken for 4 days. I am 54 years old. This is a horrible drug! Don't take it! I'm sick of these new "wonder" drugs (like Levaquin, even worse than Bioxin) that just make you worse than your illness, and I'm sick of doctors who prescribe them and then don't believe you when you have unbearable side effects. It should be taken off the market.
I have experienced some of these side effects-
Abdonimal pain, gas, bloating, depression (really severe), dizziness, "spaced out," disconnected feeling, fatigue, unable to concentrate. This drug has really messed up my week--I can't get anything done, just walk around in a daze. And my sinuses & cough aren't all that much better.
I hope this information will be useful to others,
Debra Breyan
Biaxin Side Effects